TRI Seminar Series: Immunology Mini Symposium - Immune Tolerance
Come along to the final instalment of the TRI Seminar Series for 2024. The mini symposium is centered around the theme of Immune Tolerance. The immune system is key for protecting its host against the attack of pathogens or foreign substances, but it also possesses a key mechanism to self-regulate to prevent the host itself from getting attacked by its own immune system. This symposium will showcase some of the recent progress made in this field with special guest presenter Prof Julie Zikherman (UCSF) as well as TRI based and external researchers with expertise immunology.
Date: Friday 29 November 2024
Time: 2:00pm - 4:00pm (join us for a networking afternoon tea from 1.15pm)
Location: TRI Auditorium or Zoom (Please register for Zoom login details)
REGISTER NOW

|
Dr. Zikherman received her medical degree in New York City and trained in Internal Medicine and Rheumatology in Boston. She studied antigen receptor signalling with Dr. Arthur Weiss at UCSF, where she subsequently started her independent lab. Her group is focused on understanding lymphocyte tolerance, regulation of immune responses, and autoimmunity. Recent work has focused on the role for the NR4A family of nuclear receptors in T and B cell tolerance, as well as novel mechanisms by which B cells respond to viral-like particles. She serves as Associate Chief for Basic Research in the UCSF Division of Rheumatology. Regulation of immune tolerance by the NR4A nuclear receptors The adaptive immune system is predicated on random VDJ gene segment recombination to generate enormous combinatorial diversity in the antigen receptor repertoire of developing T and B lymphocytes. However, the price of such diversity is the risk of autoimmune disease. The immune system has evolved layered tolerance mechanisms to prune and constrain self-reactivity both during and after lymphocyte development. Our laboratory is interested in dissecting these mechanisms and we have focused for several years on understanding the role of the NR4A family of orphan nuclear receptors in immune cell tolerance. The NR4As are rapidly induced by antigen receptor signalling and have tolerogenic as well as anti-inflammatory roles in various immune cell types. This presentation will focus on roles for the NR4A family in modulating mature B cell responses to antigen, and in central T cell tolerance in the thymus via deletion, Treg diversion, and anergy. These studies have translational significance as the NR4A family members may represent appealing therapeutic targets for drugs and genetic engineering to modulate immune responses in the setting not only of autoimmunity, but also vaccination, cancer, and transplant tolerance. |
|
Dr Zhian (Anthony) Chen is a senior research fellow and NHMRC Emerging Leadership fellow at the UQ Frazer Institute. He was awarded PhD in late 2017 from Monash University. His research primarily focuses on elucidating the molecular mechanisms that govern T-cell-mediated immunity, with a specific emphasis on the role of follicular helper T (TFH) cells in antibody response and the significance of TFH signature cytokines in supporting germinal centre response while preventing T cell exhaustion. Dr Chen's work employs multi-disciplinary techniques has led to several high-impact discoveries in the field. Non-canonical regulation of IL-21 bioavailability and activity controls humoral and cellular immunity Interleukin-21 (IL-21) is a crucial member of the common gamma chain cytokine family. It plays an indispensable role in both humoral and cellular immunity, notably sustaining germinal centre (GC) B cells to drive high-affinity antibody production, while also preventing CD8+ T cell exhaustion in the context of chronic infections and cancer. Traditionally, IL-21’s function is understood to be regulated by the secretion levels of IL-21 itself or through the expression levels of its receptor. Here, I present a non-canonical yet critical mechanism that modulates IL-21 bioavailability and signalling strength through a specific biochemical motif within IL-21, which interacts with non-IL-21R binding partners. B cells utilise this mechanism to attenuate IL-21 binding and signalling in GC B cells, thereby enforcing a stringent signalling threshold required for proper affinity maturation during antibody responses. Furthermore, CD8+ T cells’ interaction to human IL-21 can be targeted using a novel anti-IL-21 super-agonistic antibody designed to exploit this same mechanism, as confirmed by crystallography studies. This super-agonistic antibody can enhance anti-tumour immunity by significantly improving CD8+ T cell functionality. |
|
Ben is a MD-PhD student from UQ Medical School Clinical Scientist Training Program, currently undertaking his PhD intercalation in immunology and rheumatology in the lab of Prof Ranjeny Thomas lab at UQ Frazer Institute. He joined the lab as a medical student in 2022 and contributed to pre-clinical mechanistic studies on the pathogenesis of rheumatoid arthritis and spondyloarthropathy. His PhD project focuses on advancing the immunological basis of gut-joint axis in spondyloarthropathy. Previously, he received his Bachelor of Science in Chemistry from Emory College and research training in Biochemistry from Emory University School of Medicine, Emory University, Atlanta, GA, USA. Breaking and Maintaining Tolerance to Gut-derived Pathobionts in Spondyloarthritis In spondyloarthropathy (SpA), peripheral and axial arthritis is often associated with gut inflammation. Intestinal microbial dysbiosis occurs in SpA. The strong genetic association with HLA-B27 along with IL-23R and CARD9, and expanded CD8 TCR public clonotypes implicate innate and adaptive immunity in the autoimmune pathogenesis, but it remains unclear how gut dysbiosis, the immune system and SpA are mechanistically linked. This work builds on the SKG mouse model of SpA. After systemic β-1,3-glucan (curdlan) injection, ZAP70W163C SKG mice develop IL23-dependent SpA-like spondylarthritis, ileitis and faecal dysbiosis with enrichment in Gram-negative pathobionts over commensals, recapitulating human SpA disease spectrum. Combining traditional immunological techniques and the cutting-edge omics, Ben’s talk will highlight how the interplay between genetic susceptibility, gut dysbiosis, innate and adaptive immunity breaks intestinal tolerance and contributes to pathogenesis of spondyloarthritis. |

Gayathri M, PhD Candidate, The University of Queensland Gaya is a 3rd year PhD student from Ranjeny Thomas' lab. Her project aims to investigate circulating islet-specific T cells in T1D patients, to identify potential biomarkers of disease progression. Islet-specific Chemokine Receptors as Biomarkers of Type 1 Diabetes Progression |



 Professor Julie Zikherman, Department of Medicine, Division of Rheumatology, University of California, San Francisco (UCSF)
Professor Julie Zikherman, Department of Medicine, Division of Rheumatology, University of California, San Francisco (UCSF)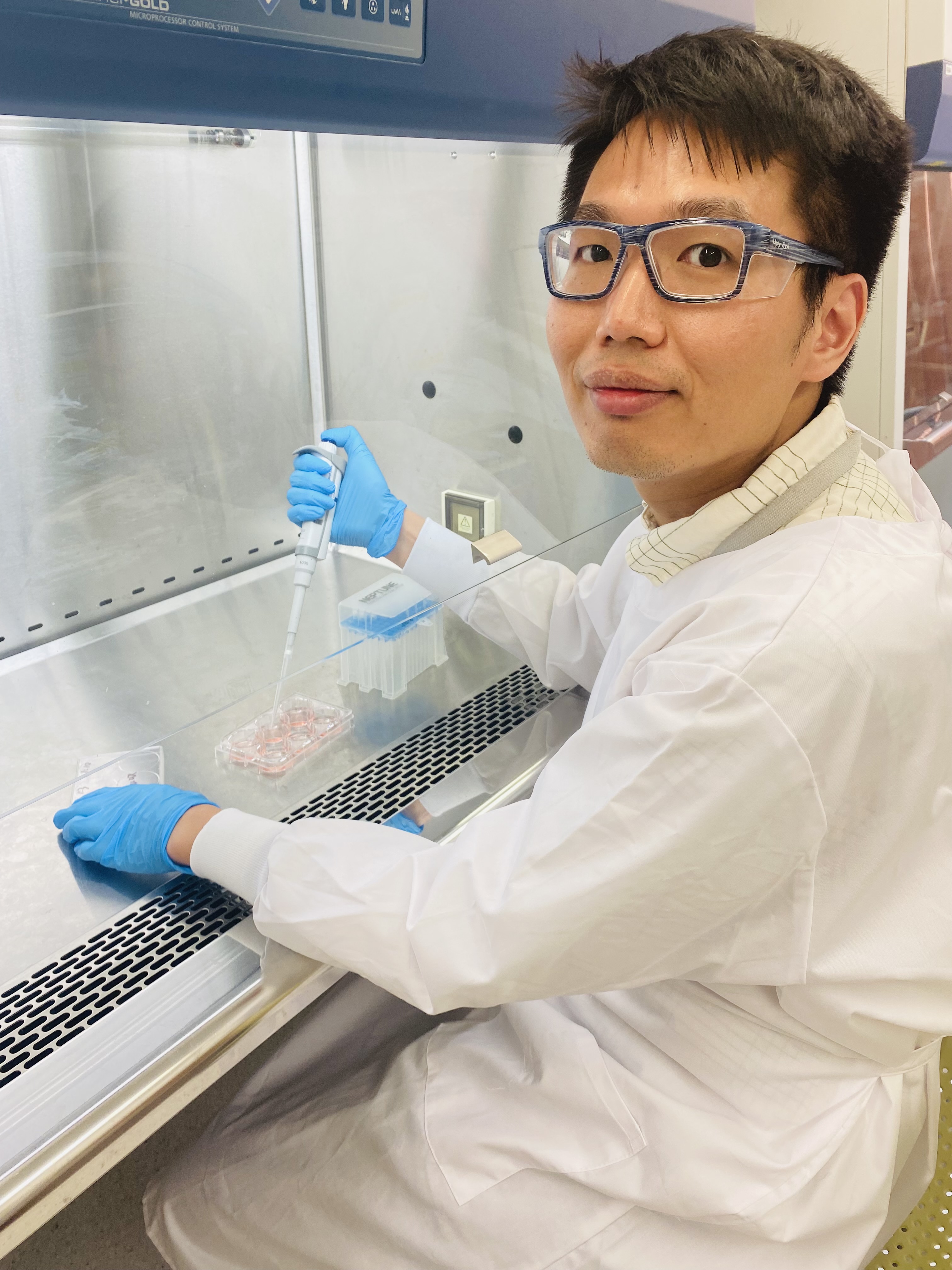 Zhian Chen, Senior Research Fellow, The University of Queensland - Frazer Institute
Zhian Chen, Senior Research Fellow, The University of Queensland - Frazer Institute Benjamin Cai, MD-PhD Student, The University of Queensland - Frazer Institute
Benjamin Cai, MD-PhD Student, The University of Queensland - Frazer Institute



