Ovarian mass - cancer or benign? A non-invasive test to triage patients before surgery
Researchers and clinicians at Translational Research Institute (TRI), Princess Alexandra (PA) Hospital and the Mater Hospital in Brisbane have teamed up to undertake a clinical trial of a non-invasive test to determine whether suspicious ovarian masses are benign or cancerous prior to surgery.
Ovarian cancer is the seventh most commonly diagnosed cancer among women in the world. There is currently no method in clinical practice to identify whether ovarian lesions are malignant, of low malignant potential or benign without the need for surgery.
“Currently, the only way to assess these lesions prior to surgery is ultrasound, as biopsy is not recommended due to the potential risk of spreading cancer cells,” says Dr Thomas Lloyd, Radiologist at the PA Hospital.
 “Depending on what is found during surgery, the patient may have the ovary removed or need more extensive surgery such as partial or complete hysterectomy. To account for this, the surgical team must plan for a wide range of possibilities, which can understandably cause patients a lot of anxiety,” explains PA Hospital Radiologist Dr Sonja Gustafson.
“Depending on what is found during surgery, the patient may have the ovary removed or need more extensive surgery such as partial or complete hysterectomy. To account for this, the surgical team must plan for a wide range of possibilities, which can understandably cause patients a lot of anxiety,” explains PA Hospital Radiologist Dr Sonja Gustafson.
“The more information we have before surgery, the better – it means we can then optimise the surgical plan for the patient, and brief them on which outcomes are more likely,” adds Natali Naude, radiographer and PhD candidate at TRI.
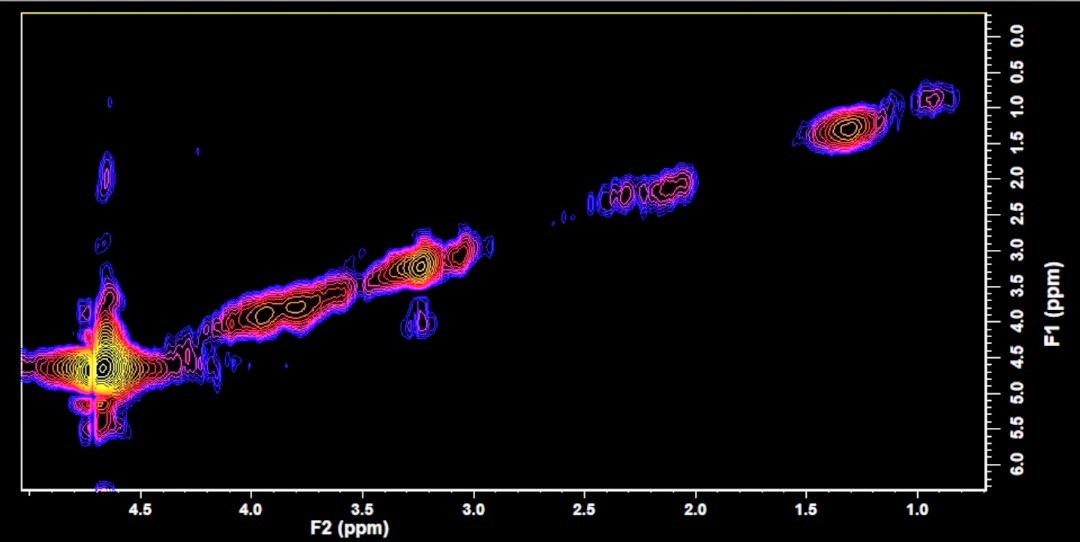
“Now, using magnetic resonance (MR) spectroscopy as a non-invasive means of evaluating tissue chemistry, we can determine if a suspicious ovarian lesion is cancerous before surgery. It is also now possible to determine whether it is a low or high grade tumour, and whether it has spread beyond the ovary,” says Professor Carolyn Mountford, CEO and Director of Research at TRI.
The technology was originally developed in Sydney at the Royal Prince Alfred Hospital and the University pf Sydney with Professors Peter Russell and Johnathan Carter. It was in regular use in 2006 as a method to triage patients, however at that time it required a physicist or PhD-qualified radiographer to operate the MRI scanner, in this case Dr Peter Stanwell.
Since then, Boston-based Professor Mountford worked with Siemens Healthineers to develop operating software that can be used by radiographers worldwide to undertake such clinical evaluations.
Using this technology, the team has commenced a clinical trial in Brisbane where the patients with ovarian masses are scanned at the PA Hospital and operated on at the Mater Hospital by Prof Lewis Perrin and his team. It is intended that the output will be data mined and classifiers developed to further automate and speed up the diagnostic process. It is anticipated that the technology with be made available worldwide by Siemens Healthineers.
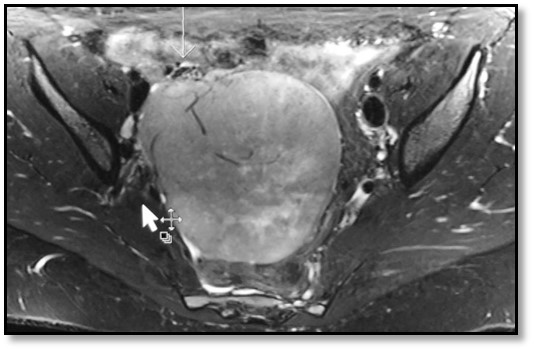
Image caption (top): Axial T2-weighted image through the mid-pelvis showing vascular infiltration into a large solid/cystic ovarian mass; (bottom) A two-dimensional reading of chemical levels in a specific area of cancerous ovarian tissue (yellow indicates higher concentrations, and blue indicates lower concentrations). These results were obtained using 2D magnetic resonance spectroscopy, obtained using a 3T Prisma MRI.







